Rebooting the Immune System by HSCT shows good results for MS patients than Beta interferon drugs
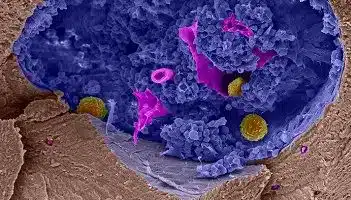
In multiple sclerosis (MS), a disease that strips away the sheaths that insulate nerve cells, the body’s immune cells come to see the nervous system as an enemy. Some drugs try to slow the disease by keeping immune cells in check, or by keeping them away from the brain. But for decades, some researchers have been exploring an alternative: wiping out those immune cells and starting over.
The approach, called hematopoietic stem cell transplantation (HSCT), has long been part of certain cancer treatments. A round of chemotherapy knocks out the immune system and an infusion of stem cells—either from a patient’s own blood or, in some cases, that of a donor—rebuilds it. The procedure is already in use for MS and other autoimmune diseases at several clinical centers around the world, but it has serious risks and is far from routine. Now, new results from a randomized clinical trial suggest it can be more effective than some currently approved MS drugs.
“A side-by-side comparison of this magnitude had never been done,” says Paolo Muraro, a neurologist at Imperial College London who has also studied HSCT for MS. “It illustrates really the power of this treatment—the level of efficacy—in a way that’s very eloquent.”
Nearly 30 years ago, when hematologist Richard Burt saw how HSCT worked in patients with leukemia and lymphoma, he was struck by a curious effect: After those patients rebuilt their immune systems, their childhood vaccines no longer protected them, recalls Burt, now at Northwestern University’s Feinberg School of Medicine in Evanston, Illinois. Without a new vaccination, the new immune cells wouldn’t recognize viruses such as measles and mumps and launch a prompt counterattack. That suggested that in the case of an autoimmune disease, reseeding the immune system might help the body “forget” that its own cells were the enemy.
Burt and others have since used HSCT for a variety of autoimmune diseases, including rheumatoid arthritis and lupus. In the past few years, several teams have reported encouraging results in MS. But only one study—which evaluated just 17 patients—directly compared HSCT to other available drug treatments.
In the new trial, Burt and his colleagues recruited 110 people with the most common form of MS, known as relapsing-remitting. In that form of the disease, patients can go long periods without symptoms—which include muscle weakness and vision problems—before inflammation flares up. Trial participants had at least two such relapses in the previous year, despite being on one of several approved MS drugs.
Half the participants continued with drug treatment but switched from a drug that wasn’t working for them to a drug of a different class. The other half underwent HSCT. First, the researchers collected their blood to reinfuse later. Then, they gave patients a combination of drugs to kill most of their immune cells. In this trial, the patients would have regenerated their own immune systems with stem cells in bone marrow that were spared annihilation, Burt notes. But they received the reinfusion of their own stem cell-rich blood to help speed recovery by several days.
A year later, the researchers evaluated how far the disease had progressed in each of the patients. According to a zero-to-10 scale of disability that includes measures of strength, coordination, and speech, roughly 25% of those in the drug treatment group showed at least a one-point worsening in their score, compared with just 2% of those in the transplant group, the researchers report online today in The Journal of the American Medical Association (JAMA).
MRI scans also revealed less extensive brain lesions in the transplant group and improvements in a patient survey about quality of life. (Survey scores worsened slightly in the drug-treated group.) Five years after treatment, about 15% of people in the transplant group had had a relapse, versus about 85% of the control group.
The two groups diverged “in a massive way,” Muraro says. But he adds that two of the most effective MS drugs weren’t included in the control group. One, ocrelizumab, had not been approved when the study was enrolling participants. Another, alemtuzumab, was excluded because it also depletes immune cells…




